Doctors vs. Denial: Taking Back Your Time and Money with Denial Management Solutions
Healthcare is both about helping people but it is also a business. Unfortunately, sometimes the latter may become rather tough. One of the major problems doctors and hospitals face is so-called ‘claim denials’. It happens when insurance companies do not pay for the service the healthcare providers have provided.
But why is it important? It simply means the doctor and the hospital are not getting money for the service. Therefore, with the development of advanced denial management solutions, healthcare systems, hospitals, and doctors get their revenue, time, and resources back. Eventually, time and money-wasting claim denials have been mitigated for salvaging healthcare practices.
The Denial Dilemma: A Closer Look
In its essence, a claim denial is the refusal of the insurance company to reimburse the healthcare provider or facility for the services provided to a patient. The reasons for such denials can vary and range from seemingly simple clerical errors, and coding discrepancies to much more complex contractual problems, and disagreements over medical necessity.
Common Culprits: Medical Billing Errors and Beyond
One of the most common causes of claim denial is a medical billing error, a problem that can take many forms. In this perspective, medical billing errors are everything from incorrect patient information, invalid insurance and policy details, and procedure codes to erroneous ICD-10 coding. Considering that the latter applies to almost every interaction with the insurance company, even a minor mistake can trigger a denial.
The denial of medically necessary treatment or service occurs if the procedure and documentation do not satisfy some of the requirements. In some cases, there can be medical billing issues, but sometimes these requirements are different. Let’s try to understand them
- Lack of Prior Authorization: Some insurance plans require pre-authorization for certain treatments or procedures. If a healthcare provider doesn’t get prior authorization before providing the service, the insurance company can deny the claim in some cases.
- Medical Necessity Disputes: Insurance companies sometimes feel that the service or treatment you gave to your patient may not be needed. Therefore, it denies it.
- Policy Exclusions: Sometimes, the paperwork may be inappropriately done. Some documents may question the service or the reason it was provided.
- Missing or Incomplete Documentation: It is common to misplace a document while filing a claim with the insurance providers. In such a case, the insurance company can deny the claim, if the necessary documents are not filed.
- Timely Filing Issues: Some insurance companies only insured services for specific periods. If any service is offered outside the stipulated interval, the insurance company will refuse any future abuse.
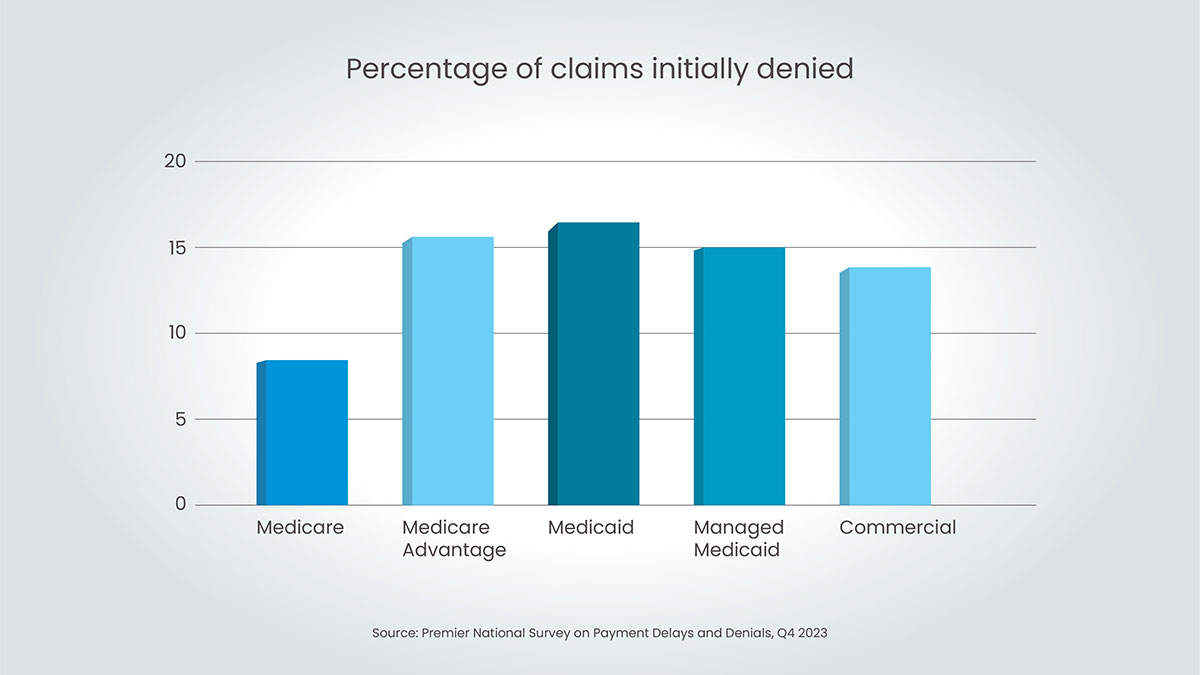
The High Cost of Denials
Denials not only result in financial losses but also require time and resources to determine and address the underlying cause. In addition to the financial dimensions affecting the healthcare provider, claims often result in unexpected expenses for patients, thus negatively affecting the relationship between the customer and the provider.
The Solution: Denial Management Solutions
Due to the spiking number of denied claims, healthcare providers decided to rely on specialized denial management services to help them overcome the current adverse effects. Using the combination of advanced technologies and the vast experience of professionals in the healthcare industry, denial management services help shape an efficient approach toward reducing denied claims. The advantages of the given approach are quite diverse:
- Reduced administrative burden: With denial management services, processing denied claims will no longer be your concern. Instead, you will be able to focus on devising comprehensive treatment approaches and managing regular clerical tasks.
- Increased revenue: More to the point, denial management services are specialists in their area; therefore, they are likely to handle denied claims with far more efficiency. Consequently, your revenue rates and revenue cycle speed will increase.
- Improved efficiency: Denial management services also provide extensive reports on the causes of denied claims as well as the changes that need to be made in your strategy for filing claims. Such an approach allows for redesigning the services so that the given problems do not occur in the future.
- Enhanced compliance: Finally, Dental management services can handle cutting-edge technology and remain updated on the latest requirements in terms of coding and billing. Get data and insights: how much are the given solutions helpful?
Key Features of Denial Management Solutions
- Denial Analysis and Appeals: Review for cause of denials and develop an effective appeal strategy. Therefore you can make sure the highest amount of reimbursement.
- AR Follow-Up: Regular follow-up to make that all claims are paid. Due to this, you decrease the non-collectibles of money.
- Claim Submission: The claim is submitted at the specified time. Hence the chance of a claim getting denied is minimal.
- Coding Review and Audit: A regular review of what codes are being applied by the providers. The errors are pointed out and the system is improved.
- Payer Negotiation: Negotiating with payers to resolve problems. Therefore increase the reimbursement by insurance companies.
By embracing denial management services, healthcare providers can transform denials from a major source of frustration into an opportunity for improvement. With streamlined processes, data-driven insights, and proactive prevention strategies, providers can reduce denial rates, improve revenue cycle efficiency, and ultimately enhance patient care.
Don’t Let Denials Win: Take Action Today
Denials are a challenge, but they’re not insurmountable. With the right tools and strategies, you can take back control of your revenue cycle and reclaim your time. Reach out to a denial management expert to see how you can start winning the battle against denials. Remember, every denied claim represents an opportunity to learn, improve, and strengthen your financial health. By taking proactive steps to address denials, you can ensure the long-term success and sustainability of your practice.
Tired of claim denials draining your time and revenue? Capline’s denial management services specialize in denial management, preventing denials before they happen, and recovering revenue on denied claims. We’ll help you navigate the complexities of insurance billing, so you can focus on what matters most – your patients.