Empowering Patients: Simplifying the Medical Eligibility Verification Process
Have you ever experienced confusion in completing medical eligibility verification? You are not alone! Understanding the details of what a patient’s plan includes can be quite a task. This situation can give a feeling of frustration to both healthcare providers as well as the staff at their office.
Why is Medical Eligibility Verification Important?
A proper analysis of your patient insurance coverage (also known as “medical eligibility verification”) ensures that you can provide appropriate care to your patients and also can get reimbursed for this. There are many more reasons why it’s important:
- Saves Money: Medical eligibility verification prevents unexpected invoices and guarantees that the patient’s insurance caters to the treatment post-medical eligibility verification. This saves money for both healthcare providers and patients.
- Faster Care: Understanding patient’s insurance ahead of time prevents hold-ups. When there are any discrepancies with the coverage, these can be resolved by the doctor’s office before patient visit.
- Fewer Errors: Confirming coverage curbs errors on bills. This helps save time for all and keeps annoyance at bay.
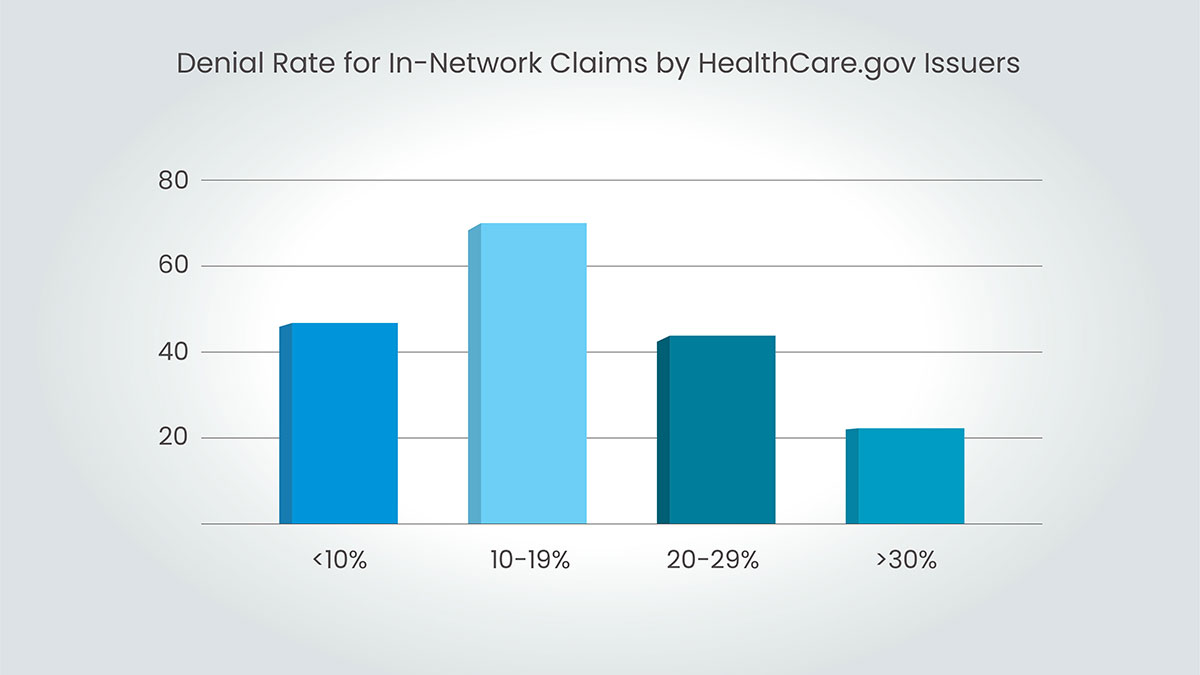
This all results in fewer claim denials, which automatically results in better reimbursement rates for healthcare providers.
The Current Challenges In Medical Eligibility Verification
Right now, checking insurance coverage can be:
- Confusing: Medical eligibility verification is very confusing. What’s covered and what’s not is hard to figure out.
- Time-consuming: The process of calling insurance companies is very time-consuming, as it causes delays in scheduling appointments and also causes barriers to providing care to patients.
- Unclear: Sometimes it’s unclear what the patient’s insurance will pay for. This can lead to undue concern about what patients might have to pay and what insurance companies might have to pay.
How Can We Make Medical Eligibility Verification Easier for Patients?
By making medical eligibility verification easier, we can give patients more control over their healthcare. Here are some ideas:
- Clear Explanations: Healthcare providers can use short videos to relay clear details about the coverage in these ways to make checking coverage easier for the patients.
- Online Tools: Online tools provide easy access to insurance eligibility information for patients. These platforms will provide the details of what medical procedures and medications are covered.
- Open Communication: Open communication channels should be established between patients, healthcare providers, and insurance firms. Engaging in discussions with patients regarding the medical eligibility verification process, possible expenses as well as their entitlements upon denial of coverage is a very good practice to follow.
Benefits of a Streamlined System
Making checking coverage easier benefits everyone:
- Happier Patients: When patients understand their coverage and costs, they feel more in control of their healthcare decisions. This leads to happier patients and better health outcomes.
- More Efficiency: A smoother medical eligibility verification process saves doctors time. This frees them up to spend more time with patients.
- Lower Costs: Less confusion and fewer errors mean less wasted money. This helps keep healthcare costs down for everyone.
Working Together for a Better System
With the establishment of a more efficient checking coverage system, technology companies in collaboration with doctors and insurance companies propose the following:
- Simpler Plans: Formats of insurance plans and summaries of benefits should be standardized; this would allow the patient to fully understand the extent of their coverage and compare plans between providers.
- Real-time Verification: It may be suggested that a technological investment allows doctors to verify patient coverage in real time while they are present at an appointment. This will decrease the delays experienced for such processes, streamline processes, and increase operational efficiency.
- Patient Tools: These are online resources and applications that provide patients with easy access to the details of their coverage and the components of the cost. These will give information about insurance terms, co-payments, deductibles, out-of-pocket payments, benefit limits, prior authorization requirements, and any other elements that determine the final sum a patient should pay.
Improving patients through a more efficient medical eligibility verification process should not burden your organization with additional tasks. Capline and its medical eligibility verification services are your partners in this journey. We employ experts in the field who take control of unraveling the complexities in coverage details— this spares your valuable staff time from mundane administrative tasks and allows them to focus on patient care (which should always be a top priority). Do you want to take that first step towards streamlining your medical eligibility verification system and also ensuring that your patients are empowered? Get in touch with Capline today for further information about what we offer!




