How to do Medical Billing
The health care industry is a web of various medical services that require administrative services to function smoothly. These administrative services include billing, charge posting, claims submission, etc. and fall under the umbrella term of medical billing. The purpose of medical billing and collection company is to optimize and enhance the revenue cycle of a hospital.
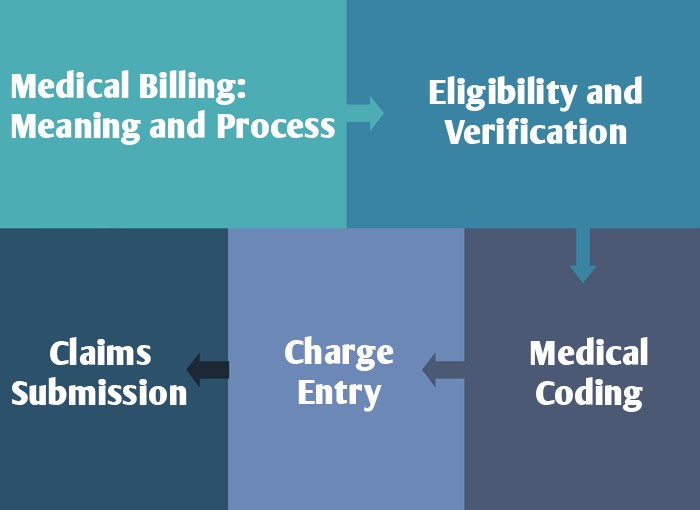
Medical Billing: Meaning and Process
Medical billing is a process focusing on three parties to boost the finances of the hospital and improve the quality of medical care facilities. The three parties in the medical billing and collection process include the patient (first-party), health care provider (second-party) and the insurance payer (third-party). While the first and second parties are very particular, the second party refers to hospitals, emergency rooms, doctors, nurses, lab tests, outpatient/inpatient facilities and medical treatments provided to the patient. These three parties are tied together to make the reimbursement process hassle-free and prevent any insurance claim denials or fraud. The medical biller is responsible to gather the information like the patient’s demographic details, health care provider’s name, medical care services provided to the patient along with their charges, and insurance payer’s details.
The medical billing process is made easy and effective by outsourcing medical billing services from medical billing companies. The medical biller provided by the company assists the hospital in generating error-free bills. The process of medical billing is as follows:
Eligibility and Verification
The step is vital in verifying the insurance claim made by the patient. This includes contacting the insurance payer (third-party) to cross the insurance details provided by the patient. This also clarifies whether or not the patient is eligible for the claim.
Medical Coding
The purpose of medical coding is to use codes assigned by medical agencies like WHO to generate a bill free from any discrepancies. The process is essential in preventing frauds that may result from up-coding or under-coding.
Charge Entry
This step is imperative in preventing denied claims. To make reimbursement successful a copy of EOB is attached to the billing sheet. The purpose is to give a detailed insight of charges to the patient as well as insurance payer.
Claims Submission
Filing insurance claims is a tricky task that requires submitting a request for claims submission by filling out a form. Nowadays, the claims submission can be done electronically.