Navigating the Maze of Medical Recredentialing: A Step-by-Step Guide
Healthcare is constantly evolving and keeping one’s credentials up-to-date is very important. The process of Medical re-credentialing helps you keep your access to insurance networks— which is very important if you want to continuously take care of your patients. Yet this process can easily overwhelm those who are already busy with providing healthcare services. This blog will take you through every step of medical recredentialing.
What is Medical Recredentialing?
During Medical re-credentialing, insurance companies and healthcare institutions regularly review your professional qualifications to verify that they are in line with their standards. It is done every two to three years, this can vary from company to company.
Why is Medical Recredentialing Important?
There are two major beneficiaries in the case of Medical recredentialing, patient and provider:
- Patient Safety: Medical recredentialing guarantees that your credentials remain up-to-date, which helps you in providing high-quality care to patients.
- Accurate Information: Medical recredentialing confirms that your license is not expired. It also checks your malpractice insurance coverage plus other essential details.
- Network Access: Remaining in-network with insurance companies is dependent on timely completion of re-credentialing— this will allow patients to receive care without increased costs.
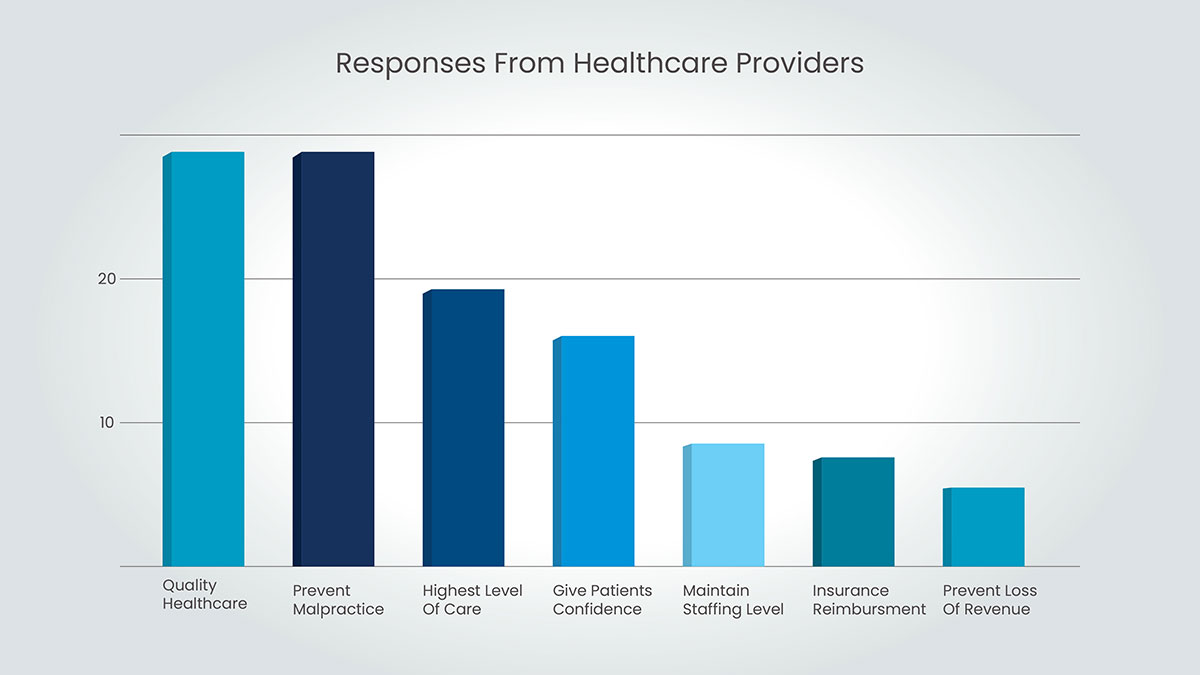
However, the importance of credentialing cannot be overstated. Still, when a survey was conducted with healthcare providers and asked why they give so much importance to credentialing or recredentialing, these were their responses:
Preparing for Medical Recredentialing
Some tips to prepare for re-credentialing effortlessly are the following:
- Stay Organized: Becoming familiar with the cycle and requirements of your re-credentialing process at your facility can be beneficial for you. For most institutions, this information should be provided during orientation or easily accessible through your medical staff office.
- Track Deadlines: You will receive notifications from insurance companies and healthcare facilities concerning the approaching re-credentialing deadlines. The significance of medical credentialing deadlines must be addressed; failure to adhere can result in loss of network access which, in turn, hampers patient care.
- Gather Required Documents: Each organization will have specific requirements. Be prepared to submit documents like:
- Updated license information
- Current malpractice insurance coverage
- Proof of Board certification (if applicable)
- Updated CV or resume
- CME certificates
The Medical Recredentialing Process: A Step-by-Step Guide
- Receive Notification: Insurance companies always send a notification that gives complete details of the re-credentialing process and deadlines.
- Review Requirements: Please make sure you followed all the requirements and have all the needed documents:
- Complete Application: Fill out the application form and always double-check every bit of information in the form.
- Gather and Submit Documents: Collect all the documentation mentioned in the guideline and share them with the insurance company.
- Verification Process: They will check all the given information with primary sources like licensing boards and,other relevant agencies..
- Decision Notification: You will get notified of the re-credentialing result. If you handed in everything correctly and on time, the result should be positive.
Tips for a Smooth Medical Recredentialing Experience
- Start Early: Don’t wait until the last minute. Begin gathering documents well before the deadline.
- Be Organized: Having a system for storing your credentials will save you time and frustration during re-credentialing.
- Read Instructions Carefully: Pay close attention to the specific requirements outlined by each organization.
- Ask Questions: If you’re unsure about anything, don’t hesitate to contact the re-credentialing department of the insurance company or healthcare facility.
- Keep Copies: Maintain copies of all submitted documents and the final re-credentialing decision for your records.
Following these steps while keeping organized will help you through the Medical re-credentialing. Furthermore, it is always vital to keep up to date since the re-credentialing process must be completed on time to ensure you still have access to the client. In other words, re-credentialing must be completed on time to ensure your patients continue to receive high-quality care.
Running re-credentialing in-house consumes much time and is quite a complicated process. Capline’s re-credentialing service’s team of specialists ensures the re-credentialing process-free for use. Our specialist team conducts the entire process by gathering your documents and documentation production and submission and communicating with the insurance companies. Therefore, you can concentrate on taking care of patients as Capline guarantees your services without any interruption due to the re-credentialing process.